-
Former California Dentist Tony Protopappas Who Killed Three Patients Is Paroled

Former dentist Tony Protopappas
Tony Protopappas came up for parole in December but former California Governor Arnold Schwarzenegger rejected it. He was ordered released by the Fourth district Court of Appeal in June.A former Costa Mesa dentist who served more than a quarter of a century in prison for murder after three of his patients died in his dental chair from improper use of anesthesia in the 1980s was paroled from Folsom Prison Tuesday.
Tony Protopappas, who made national headlines in the early 1980s when he was convicted of three counts of second-degree murder, was picked up by his brother at the gates of Folsom Prison shortly after 9 a.m. Tuesday, said Santa Ana attorney Rich Pfeiffer, Protopappas’s appellate lawyer.
“He was very, very thankful,” Pfeiffer said. “He was crying tears of joy.”
Protopappas was ordered released on parole in June by the Fourth District Court of Appeal in June in a ruling that overturned a decision by former Gov. Arnold Schwarzenegger in 2010. Schwarzenegger reversed a decision by a state parole board granting Protopappas’ release because he no longer presents a risk of danger to others.
Pfeiffer then appealed Schwarzenegger’s reversal, insisting that there is no evidence that Protopappas is an unreasonable risk to society, Pfeiffer said Protopappas should have been released from prison last week under the appellate decision, adding that he has filed a writ seeking to hold prosecutors in the state attorney general’s office in contempt of court for not allowing the former dentist to be released on time.
Protopappas is now 65 years old and will NEVER practice dentistry again. But, three patients are dead and will have no life, because of his grossly negligent conduct.
Granted he never intended to kill his victims, but he did, and for that he deserves to spend the rest of his life in prison.
California Governor Arnold Schwarzenegger Rejects Parole for Deadly Dentist Tony Protopappas
-
Video: Oregon Woman Wakes Up After Oral Surgery Sedation With a British Accent
Visit msnbc.com for breaking news, world news, and news about the economy
The strange case of Karen Butler.
Karen Butler has a British-sounding accent, but she’s never been to Europe. She woke up from dental surgery one day talking funny. A year and a half later her “foreign” accent remains, and her story has traveled around the world.
The 56-year-old tax consultant from Toledo, Ore. has found her life transformed by the dental procedure, which left her with dentures, and – depending on whom you ask – an Eastern European, Swedish or British accent.
Butler had all her top teeth and front bottom teeth removed in November 2009 because of gingivitis. A week later the swelling had gone away, but she still sounded strange. Her dentist told her she just had to get used to her new teeth.
But as weeks stretched on with no change, Butler did some online research. She diagnosed herself with Foreign Accent Syndrome, a medical condition with only a few dozen documented cases.
The syndrome is often the result of brain injury; though it is uncommon, most neurologists will see at least one case in their career, said Dr. Helmi Lutsep, professor and vice-chair of the Department of Neurology at Oregon Health & Science University. Sometimes a person just sounds slightly off; other times there may be a more dramatic-sounding accent, Lutsep said.
“We don’t know exactly how or why it happens, but it simply affects rhythm of language,” Lutsep said. “I’m absolutely convinced this is a real phenomenon. These people are not making it up.
Wow! I wonder if she will have any other concomitant complications.
It will be interesting to follow this case.
-
Oral Hygiene and Antibiotics Play a Role in Healing and Pain Alleviation in Bisphosphonate-Related Osteonecrosis of the Jaw (BRONJ)

Osteonecrosis of the jaw in a patient who had poor oral hygiene and generalized periodontal disease and recently underwent routine dental extractions in the mandible. This patient had undergone monthly intravenous bisphosphonate therapy for treatment of multiple myeloma during the previous 12 months.
Photo credit: Mayo ClinicAccording to this new paper here.
Abstract
OBJECTIVES:
The objectives of this study were to define the incidence, pain, and healing in cancer patients treated with intravenous bisphosphonates.
STUDY DESIGN:
The study included long-term follow-up of 99 bisphosphonate-using patients (group A) and conservative treatment of 67 patients with bisphosphonate-related osteonecrosis of the jaw (BRONJ, group B) using 3 antibiotic schemes and oral hygiene.
RESULTS:
The frequency of zoledronic acid single-agent use was 85.9% and 69.8% in group A and B, respectively. Median follow-up was 13 months (group A) and 16 months (group B). Two patients in group A developed BRONJ (2%). Of those with BRONJ in group B who completed follow-up, healing occurred in 14.9% (7/47) and pain subsided in 80.9% (38/47). Healing was significant in patients who received pamidronate followed by zoledronic acid (P = .023) and with BRONJ stages 0 and stage I (P = .003).
CONCLUSIONS:
This case series suggests that oral hygiene and conservative antibiotic therapy play a role in healing and pain alleviation in BRONJ. Oral hygiene and follow-up may decrease incidence of BRONJ.
This sounds a reasonable course, knowing that this complication will be found to occur with increasing frequency. Let us hope a conservative protocol can be developed for these unfortunate patients.
Previous:
Jury Finds Novartis the Manufacturers of Zometa Not Liable for Osteonecrosis of the JawOral Bisphosphonates: Study – Absolute Risk for Femur Fracture Low with Bisphosphonates
Revisiting Bisphosphonates and Femur Fractures
New Dentistry Cause for Alarm for Patients Who Use Bisphosphonates – Fosamax, Actonel, Boniva?
-
Jury Finds Novartis the Manufacturers of Zometa Not Liable for Osteonecrosis of the Jaw

Osteonecrosis of the Jaw (ONJ)
Another bisphosphonate law suit.A U.S. federal jury found that a bone drug made by Novartis Pharmaceuticals Corp was not to blame for the severe jaw deterioration developed by a Rhode Island man who died of cancer in 2005.
Karleen Hogan, the widow of Timothy Hogan, claimed in a lawsuit filed in 2006 that Novartis had failed to properly warn her husband about the severe adverse effects caused by Zometa, a drug used to strengthen bones in cancer patients. She sought compensatory damages for her husband’s suffering.
The suit is one of an estimated 600 filed against the unit of Novartis AG in recent years blaming the company for suppressing information about adverse effects linked to Zometa and Aredia, another bone-strengthening drug.
I think what helped the defendants in this case was the testimony from the patient’s physican and dentist who said he had pre-exisiting dental problems and that the benefits of the drug outweighed the risks.
But, there is a mixed record on these suits and there will be more to come.
Hogan’s case was initially consolidated with hundreds of Zometa and Aredia liability suits in multi-district litigation in Tennessee federal court. Similar litigation is also pending in a state court in New Jersey.
Hogan’s is the fourth Zometa case to go to trial. In October 2010, a New Jersey superior court jury ruled in favor of Novartis. A jury in Montana state court awarded a plaintiff with the same jaw disease $3.2 million in October 2009, and in November, a federal jury in North Carolina awarded a North Carolina woman’s family $12.8 million, later reduced to $1.26 million.
Osteonecrosis of the Jaw Associated With Bisphosphonate Agent Zoledronic Acid and Chemotherapy Combined With the Antiangiogenic Agent Bevacizumab
Oral Bisphosphonates: Study – Absolute Risk for Femur Fracture Low with Bisphosphonates
Revisiting Bisphosphonates and Femur Fractures
New Dentistry Cause for Alarm for Patients Who Use Bisphosphonates – Fosamax, Actonel, Boniva?
-
Florida Dentist Arrested After Fighting 85 Year Old Patient Over Her Dentures

Dental Patient Virginia Graham – click on photo for video
Good grief, what a moron.A Florida dentist is facing assault and battery charges after he allegedly tussled yesterday with an 85-year-old patient over her dentures, police report.
According to cops, Michael Hammonds, 57, was attempting to adjust Virginia Graham’s “lower partial dentures” when the senior citizen “began screaming” due to pain caused by the ill-fitting false teeth.
“Graham removed the partials from her mouth and threw them at Hammonds, which he caught,” according to a Volusia County Sheriff’s Office report.
When Hammonds refused Graham’s demand for a $900 refund, she tried to snatch the dentures from the dentist’s hand, prompting a “brief tug-of-war.” At that point, “Graham then bent down and bit Hammonds hand forcing him to let go of the partial.”
Graham then got out of the operating chair and sought to leave Hammonds’s Deltona office. But the dentist “got in her face and began screaming at her, causing her to fear that he would potentially cause her harm,” investigators reported. Graham told deputies that Hammonds physically kept her from leaving his office. She “made one final attempt to leave by trying to climb over the receptionist desk and out the receptionists window,” but abandoned that bid in order to avoid injury.
Sheriff’s deputies observed “multiple bruising” on Graham’s upper arms and forearms, and her “left upper arm was bleeding due to her skin tearing when Hammonds grabbed her arm.”
Investigators–citing the “totality of the circumstances of Graham being 85 years of age” and “Hammonds depriving her the free will” to leave the office–arrested the dentist on a variety of felony charges, including assault, battery, and false imprisonment.
Hammonds was booked yesterday afternoon into the Volusia County jail, and later released after posting $4000 bond.
Here is a photo of the dentist, Dr. Michael Hammonds:
 The dentist as it turns out has a history of violence according to some of his patients.
The dentist as it turns out has a history of violence according to some of his patients.Aniseto Morales and his wife went to Elkcam Dental back in November after a crown they paid $1,300 for broke. They say the dentist office would not fix the work that was only a few months old. And the couple claims they were suddenly attacked by Dr. Hammonds.
“He came running out like a maniac, grabbed him by the neck and, I’m scared,” said Gladys Morales, patient’s wife.
WFTV spoke with another person who said he was verbally assaulted by the dentist and then pushed out of the office, while he was on crutches.
Neither incident had enough evidence to warrant criminal charges, but they have all come forward after they saw what happened to 85-year-old Virginia Graham.
His dental license has also been suspended in the past.
Dr. Michael Hammonds has been suspended for performing an improper root canal, failing to provide proper dentures to a patient, and then in 1997 he was sentenced to 33-months in prison for 10-counts of tax evasion. His license is currently active.
Here are links to State of Florida, Department of Professional Regulation, Board of Dentistry:
I don’ think Dr. Hammonds will be practicing dentistry in Forida or anywhere after he finishes his incarceration.
-
Twin American Dentists’ Path Leads to Iraq

Army Capts. (Drs.) Aleksandr Baron and Dmitry Baron stand together outside of the dental clinic at Contingency Operating Site Kalsu, Iraq, May 6, 2011. The twin brothers are augmenting 3rd Armored Cavalry Regiment in southern Iraq. U.S. Army photo by Spc. Maksim Shchekoturov
Suffering from a toothache in southern Iraq may land you in the chair of either of two brothers with an interesting story of adversity, perseverance, and the unique bond of identical twins.
Army Capts. (Drs.) Aleksandr and Dmitry Baron both serve in the 3rd Armored Cavalry Regiment as dentists on separate bases in southern Iraq. Both are augmenting the unit from their home base of Fort Stewart, Ga. Aleksandr deployed to Contingency Operating Site Kalsu at the end of October to work with the Regimental Support Squadron, and Dmitry joined the regiment’s 3rd Squadron at Contingency Operating Site Echo in April.
Both men volunteered for the deployments, but Dmitry’s recent arrival to the same unit in Iraq was mere coincidence, the kind of common occurrence that has kept these twins together for most of their lives. The tight bond between them was forged when their parents, Vitaly and Emma Baron of Aberdeen, N.J., decided to take them from Russia to America when they were 6 years old.
Read it all.
Thank you gentlemen for your service!
-
Pew Center: The State of Children’s Dental Health – California’s Report Card
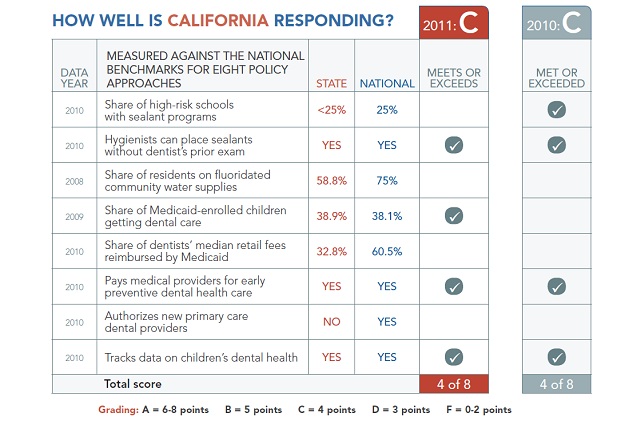 A grade of “C” from the Pew Center on the States.
A grade of “C” from the Pew Center on the States.California meets half of the eight policy benchmarks for improving children’s dental health, but children in the state still face significant barriers to accessing care. A recent study by Children Now revealed that one in five California children under age 12 had never seen a dentist. To help alleviate this problem, stakeholders in the state are exploring innovative ways to expand the dental workforce. Pew is supporting a campaign in California to authorize a new type of dental provider who can offer primary care.
Although the state does not yet meet the benchmark for water fluoridation, it has improved significantly since 2006, with over half of the state now receiving the benefits of fluoridated water.
I have some problems with the criteria the Pew Center uses to judge the state of children’s dental health and really see little correlation between each of the categories to judge an overall state of health.
Let me take them one at a time.
Share of high-risk schools with sealant programs:Pew is assuming that more dental sealants mean better dental health. Over the 30 years of placing and evaluating dental sealants, I have seen little reason why having a school program in high-risk disadvanatged area would correlate to better dental health. Just because there is a program and sealants are placed, does this mean less decayed and missing teeth as adults? I would like to see a current model and study.
Hygienists can place sealants without a dentist’s prior exam:
What does this have to do with children’s dental health? Some states allow this and some don’t – big deal. How difficult is it for a school or public health based clinic to have a retired licensed dentist or dentist volunteers to at least examine the children. Or, does hygienist placement of sealants without a dentist examination mean a better outcome? This is hard to believe.
Share of residents on fluoridated community water supplies:You might expect better dental health with fluoridation. But, what abut the communities that have naturally fluoridated water? And, isn’t this really a political decision by the local communities and not the states?
Share of Medicaid-enrolled children getting dental care:More Medicaid children seeing a dentist probably means better dental health. But, what type of treatment are they receiving? Extractions, restorations or regular preventive care? Do the patients return on a regular basis? And, do the states really want to promote utilization of their resources to Medicaid recipients by marketing? I would guess not.
Share of dentists’ median retail fees reimbursed by Medicaid:
Dentists receiving more of their regular fee for treating Medicaid children might mean more dentists treating more children, right? Yes and No. Some dentists don’t participate in Medicaid regardless of the fees paid, because of the needless bureaucracy and ever present/relentless federal audits which might send them to prison for making billing errors. Some dentists just don’t like the federal government intruding on their private business decisions. So, increasing the fees for Medicaid might reward some dentists, but probably would not increase the numbers of dentists providing Medicaid treatment – unless of course, the fees approached 80-85% of their UCR. But, what states and which taxpayers will be able to afford that?
Pays medical providers for early preventive dental health care:I cannot imagine seeing general/family practice physicians, pediatricians or PA’s sitting down in a Medicaid environment either providing dietary advice, dental sealants, or oral hygiene instructions. Just because physicians can, does not mean most M.D.’s will. I would like to see a study as to which states have a goodly number of M.D.’s providing these type of services.
Authorizes new primary care dental providers:
This is, of course, the hidden agenda question for the Pew Organization who has been at the forefront in promoting the new dental therapist as an alternative to the dentist. This category has no relevance to children’s dental health, since there is no evidence that having dental therapists equates to better dental health. Most of the USA is not Alaska, remote and rural. I don’t think most private practice dentists are going to hire dental therapists, so they can see more Medicaid patients with a reimbursement of around 40% of their regular fees. Remember the “invisible hand?”
Tracks data on children’s dental health:
More government bureaucracy reporting to the federal government really equates to better dental health.
As you can see, I am not too fond of this report. But, Pew is a large, well-funded organization and one with an agenda to promote dental therapists as a way to improve access to dental care for underserved populations. This report must be viewed with this in mind.
Here is the last graph on California’s report card:
-
President 2012: Is Tim Pawlenty A Friend of Dentists?

Republican Minnesota Governor Tim Pawlenty announces that he is running for President in Des Moines, Iowa, May 23, 2011
The legislative battle over what have come to be known as “midlevel providers” in Minnesota has come to a close.
What began as two distinct models of education and practice emerged as one with the state creating a new position—the dental therapist—who will provide care for underserved patient populations in the state.
Gov. Tim Pawlenty signed Senate File 2083 May 16, creating the dental therapist, a licensed provider with a bachelor’s degree in dental therapy who will work with Minnesota-licensed dentists to provide preventive dental services, restoration of primary and permanent teeth, extraction of primary teeth and select other dental treatments.
Governor Pawlenty signed the legislation and now will be held accountable. Pawlenty is not a fan of dentistry no matter how the American Dental Association or anyone else spins it. He could have vetoed the legislation.
Dental therapists or mid-level providers will fracture American dentistry into multiple tiers of care and help undermine private practice while increasing Big Government control of my profession.
Sorry, Tim. I will support and vote for someone else.
-
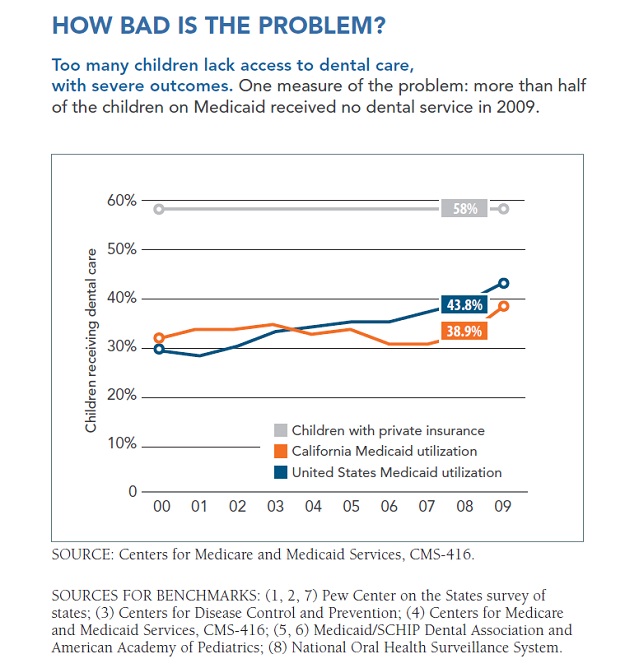
Pew Center: The State of Children’s Dental Health
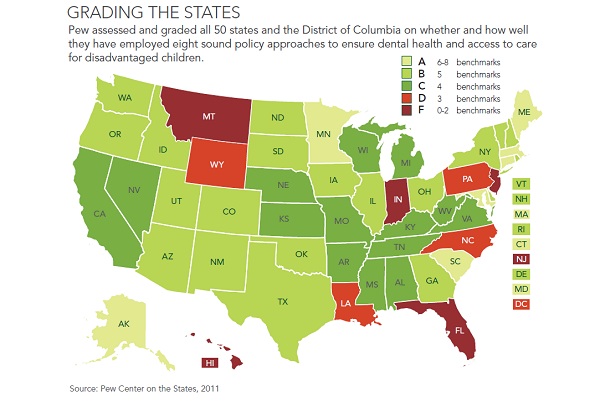 The Pew Center on the States is up with their latest state grades on children’s dental health.
The Pew Center on the States is up with their latest state grades on children’s dental health.More than 16 million children still lack access to basic dental care despite efforts by states to improve their dental health policies, according to this year’s 50-state report card from Pew.
The State of Children’s Dental Health: Making Coverage Matter graded states’ ability to serve insured and soon-to-be insured children. In the face of major budget shortfalls, 22 states were able to raise their 2010 grades, proving that dental health policies can be improved at a relatively low cost.
Pew graded the states based on eight benchmarks that are a roadmap for policymakers looking to improve and expand access to children’s dental health. The grades reflect changes that have occurred since Pew’s initial assessment in 2010.
While many states have made significant strides in improving oral health policies, too may kids children without proper dental care, mainly because of a shortage of dentists willing to serve Medicaid-enrolled patients.
I will have more to say on their report in the morning, but for now, here are the key findings.
- 27 states earned grades of an A or B, while 23 states and the District of Columbia received a C or lower grade.
- 22 states raised their grades and six of them have improved by at least two letter grades: Arkansas, Delaware, Massachusetts, Minnesota, Utah and West Virginia.
- Seven states received an A grade, and five earned an F. Three of those five states—Florida, Hawaii and New Jersey—got an F for the second consecutive year.
- States that raised their grades made progress primarily by reimbursing physicians for preventative dental services, expanding water fluoridation and increasing the percentage of Medicaid-enrolled children who receive care.
- 23 states made no progress over last year’s grades.
- Six states received lower grades mainly because Medicaid reimbursement rates have not kept pace with the growth in dentists’ fees.
California received a grade of “C” which is surprising due to the fact that the state eliminated Dental Medicaid for adults. But, I suppose this is a children’s report. I will discuss the methodology and their findings tomorrow.
-
Osteonecrosis of the Jaw Associated With Bisphosphonate Agent Zoledronic Acid and Chemotherapy Combined With the Antiangiogenic Agent Bevacizumab

Osteonecrosis of the Jaw (ONJ)
This study has just appeared in the Journal of the American Dental Association. Here is the abstract.Background. The authors investigated the incidence of and risk factors for osteonecrosis of the jaw (ONJ) in patients with metastases to the bone who received the bisphosphonate agent zoledronic acid (ZOL) and chemotherapy combined with the antiangiogenic agent bevacizumab (BEV).
Methods. The authors evaluated 59 participants (34 with breast cancer and 25 with nonsmall-cell lung cancer). All of the participants received 4 milligrams of ZOL via intravenous (IV) infusion every four weeks and 15 mg per kilogram of BEV every three weeks. They conducted a dental examination in participants at baseline and every three months until the patients died or were lost to follow-up. If needed, participants received periodontal disease treatment and underwent tooth extraction before they started receiving ZOL and BEV.
Results. The median time the participants received ZOL therapy was 18.8 months (range, 3.1–28.9 months); 36 participants (61.0 percent) received ZOL therapy for more than one year. The median time participants received BEV therapy was 16.7 months (range, 2.8–29.6 months). None of the participants required dentoalveolar surgery while undergoing cancer treatment. After a median follow-up period of 19.7 months, none of the participants developed bisphosphonate-related ONJ.
Conclusions and Clinical Implications. ZOL combined with BEV did not predispose to ONJ participants with cancer that had metastasized to the bone who underwent a baseline dental examination and preventive dental measures. The study results must be considered in the context of the study’s protocols and the follow-up period.So, the question is whether these patients were prevented from developing osteonecrosis of the jaw (ONJ) because of the drug therapy or because of dental treatment protocols?
The researchers took several measures to reduce the study participants’ risk of developing ONJ, including the following:
- Dental caries and periodontal disease were treated before starting study treatment.
- Mouth rinses with chlorhexidine and local antibiotic agents were administered before baseline oral hygiene.
- Recommendations were made for maintaining good oral hygiene.
- Teeth were extracted at least four weeks before starting ZOL and BEV therapy.
- Invasive dental procedures were avoided during treatment.
- If invasive dental procedures were needed during treatment, ZOL and BEV were readministered after at least four weeks.
All the patients received a dental exam and panoramic x-rays before starting treatment and every three months until the patients died or were lost to follow-up. After a median follow-up period of 19 months, none of the study participants had developed ONJ.
So, antiangiogenesis or treating the patient dentally prior to IV ZOL treatment?
The jury continues to be out.
But, preventive dental measures, including baseline dental examinations and follow-up are simple to institute and probably prudent, in any case.
“Although further research is needed, the results of our study suggest that ZOL combined with the antiangiogenic agent BEV does not predispose patients with metastases to the bone from breast and NSCL cancer to ONJ if they undergo a baseline dental examination,” they concluded. “Nevertheless, the results of the study must be considered in the context of the follow-up period used in the study and the use of the preventive dental protocol.”
Tanja Fehm, MD, from the department of obstetrics and gynecology at the University of Tübingen in Germany, has done similar research (Gynecologic Oncology, March 2009, Vol. 112:3, pp. 605-609). She told DrBicuspid.com that the incidence of ONJ is low — between 1% and 4% — in metastatic breast cancer patients receiving bisphosphonates.
“Therefore, the number of patients (59) investigated in this study is too low to make meaningful conclusions,” she added. “However, the paper summarizes the preventive measures that can help avoid ONJ.”
Previous:
Oral Bisphosphonates: Study – Absolute Risk for Femur Fracture Low with Bisphosphonates
Revisiting Bisphosphonates and Femur Fractures
New Dentistry Cause for Alarm for Patients Who Use Bisphosphonates – Fosamax, Actonel, Boniva?